Comfortably numb: The history of local and regional anaesthesia
The Anaesthesia Museum’s temporary exhibition for 2020 focuses on local and regional anaesthesia. As the museum is currently closed due to COVID-19, we have made it accessible online. Do come and visit us when we re-open to explore the objects on display which tell the story of this aspect of anaesthesia.
A selection of objects on display
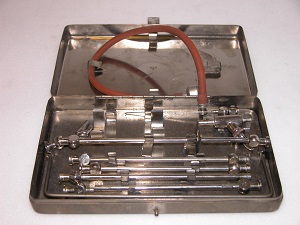
Nerve stimulator

To confirm the correct placement of the needle tip, nerve stimulators were introduced. A low electrical current is passed down the needle to stimulate the target nerves and cause a ‘twitch’ in the muscles it supplies. To ‘see’ where the nerve is, an ultra-sound device can be used.
Novocaine
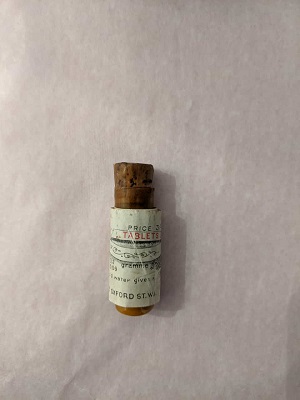
Novocaine decays when in solution so clinicians used the tablets to make up a fresh solution just before use.
Courtesy of Thackray Medical Museum.
Glass hypodermic syringe

Early syringes were ill-suited for the administration of regional anaesthesia. The Record Syringe, introduced in 1906, was one of the first glass and metal syringes that was highly dependable and easy to take apart for sterilisation.
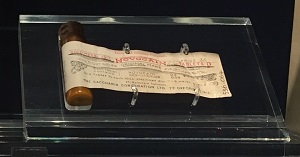
Labat spinal set and Labat syringe

Introduced by Gaston Labat in 1922, one of the pioneers of regional methods, this spinal set contained a syringe and a needle that were specifically developed for the administration of regional anaesthesia.