A bloodless field for surgery: Induced hypotension - a blog post from the Heritage Centre
Induced or controlled hypotension (low blood pressure), which was introduced into anaesthetic practice in the late 1940s, required a new way of thinking for the anaesthetist. Before then, an anaesthetist was trained to maintain blood pressure at the ‘normal’ level. The idea of reducing blood pressure to a point where it was not recordable in the usual way with a blood pressure cuff seemed nonsensical. Add to that, the fact that this technique was being used on patients with high blood pressure and therefore at higher risk of coronary heart disease and stroke, and the practice seemed reckless.
However, induced hypotension extended the range of surgeries and was utilised in major operations where there was significant blood loss, or where there was a risk of rupturing a blood vessel (e.g. aorta operations). It also provided a greater understanding of body systems, which improved ways on controlling the body to improve patient safety.
Monitoring blood pressure has been one of the earliest forms of monitoring by anaesthetists. First used during anaesthesia in 1901 by American surgeon Harvey Cushing. Joseph Clover was the first exponent of pulse measuring in the late nineteenth century.

Clover with his chloroform apparatus, 1862

Dr Harvey Cushing
Blood pressure monitoring techniques can be traced back to the eighteenth century. The first machine for measuring and recording blood pressure came in 1860. Advancements to these early techniques and equipment have been made since that first measurement of blood pressure in 1733.
The first person to quantitatively measure blood pressure was Stephen Hales. He was a physiologist, clergyman and one of the most famous British scientists of his day. His investigations at Corpus Christi College, Cambridge into arterial systems in animals were published in, Statistical Essays: Containing Haemotaticks in 1733. In these investigations, he inserted a manometer (glass tube filled with mercury) into the artery of a horse and measured the height the blood rose, and so the first measurements of blood and pulse pressure were made.
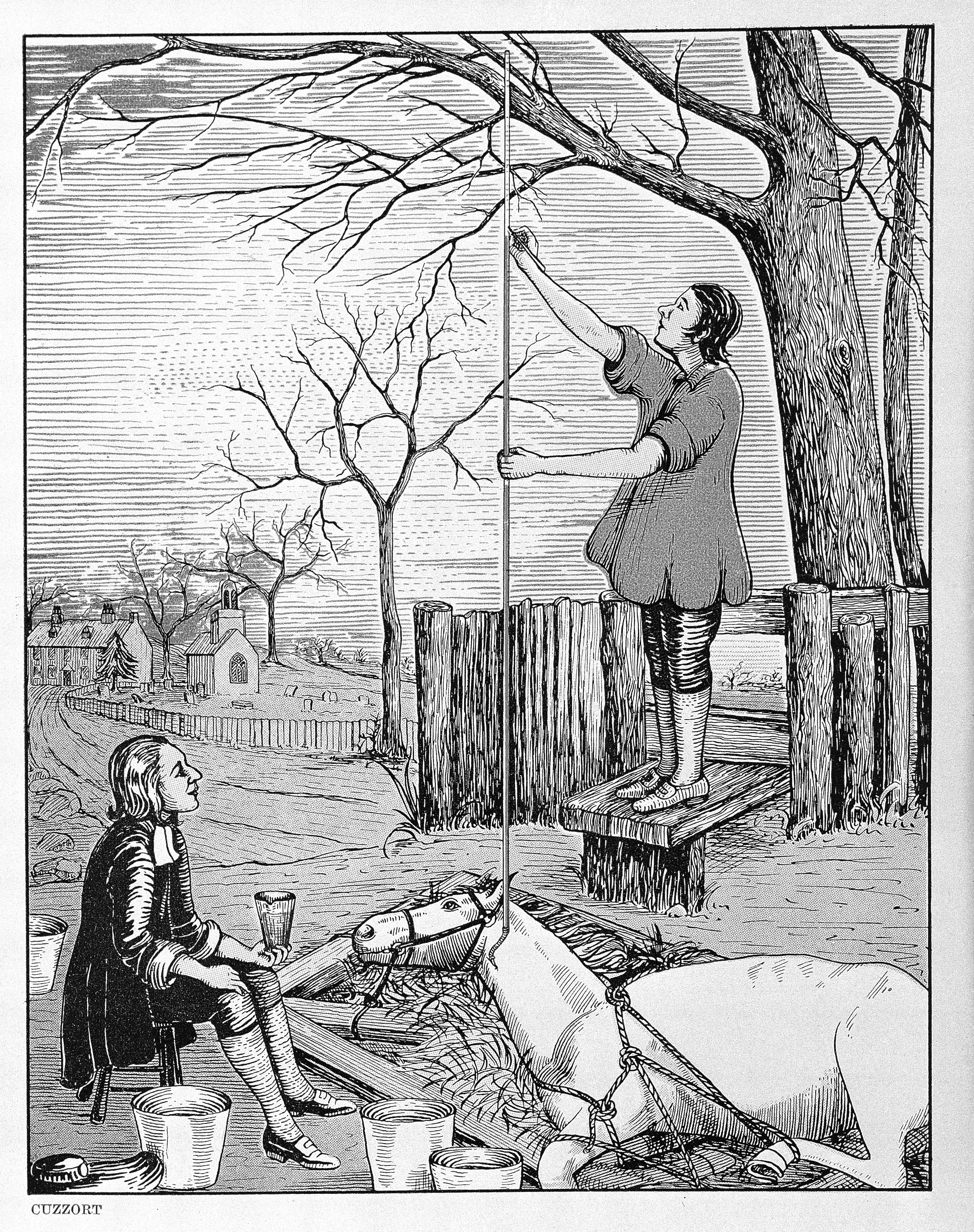
Hales' Horse. Image credit: Wellcome Collection
The next advancements were made by French physician and physiologist Etienne-Jules Marey whose 1860 ‘Marey Sphygmograph’ was the first instrument of its kind to be widely used in clinical medicine. It produced a paper record of blood pressure. The sphygmograph was held on the patient's forearm with a cloth band and an ivory plate was positioned on the patient's radial artery. The patient’s pulse created a motion which was transmitted through a stylus dipped in ink and onto a piece of paper, thereby creating a line which represented the motion.
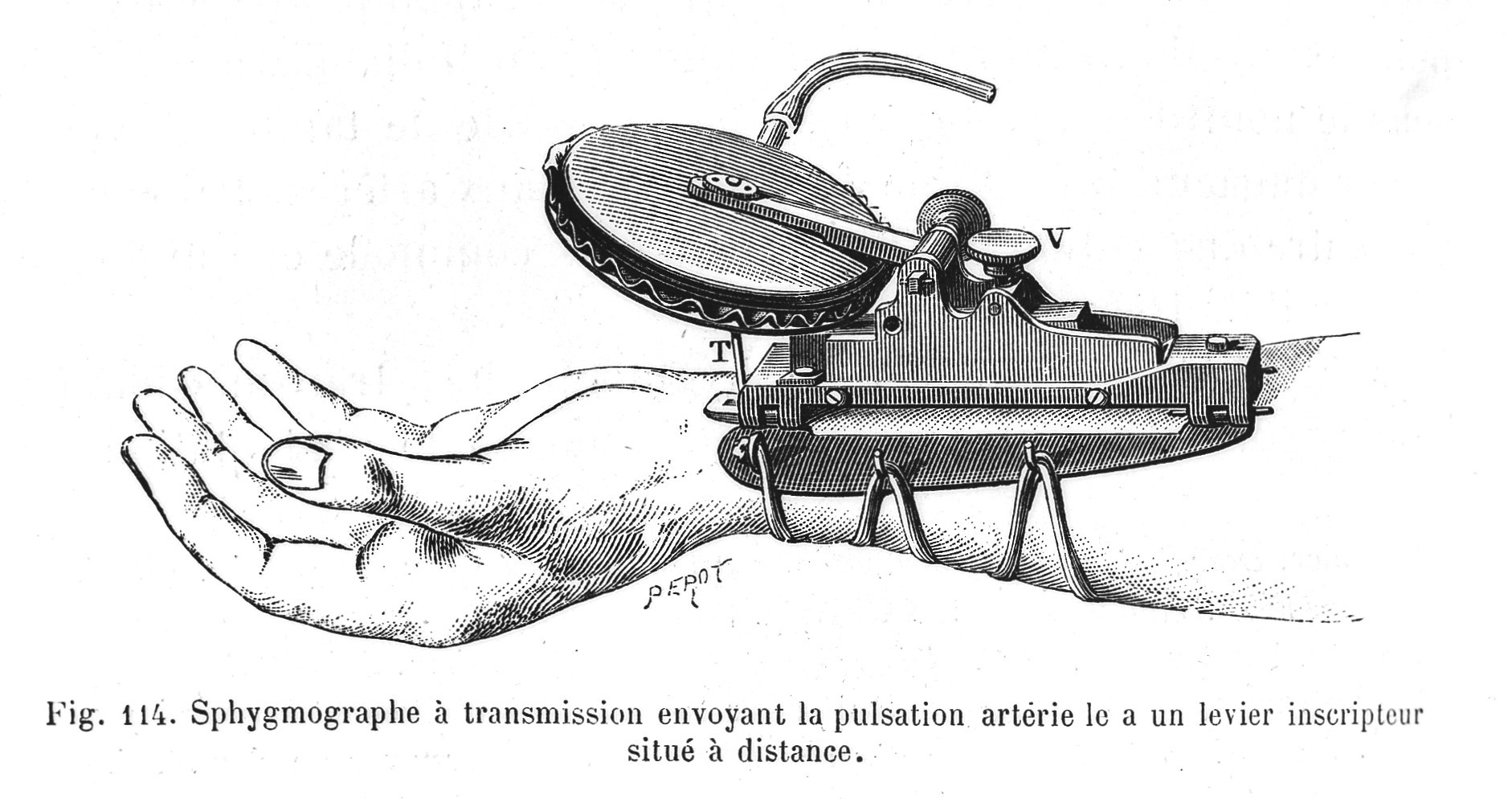
Illustration of Marey Sphygmograph. Credit: Wellcome Collection
The first sphygmomanometer was invented in 1881 by Austrian physician Karl Samuel Ritter von Basch. The manometer included a small balloon and a dial. The balloon was placed over the artery in the wrist and compressed until the pulse disappeared. The pressure needed to do this was then read on the dial.
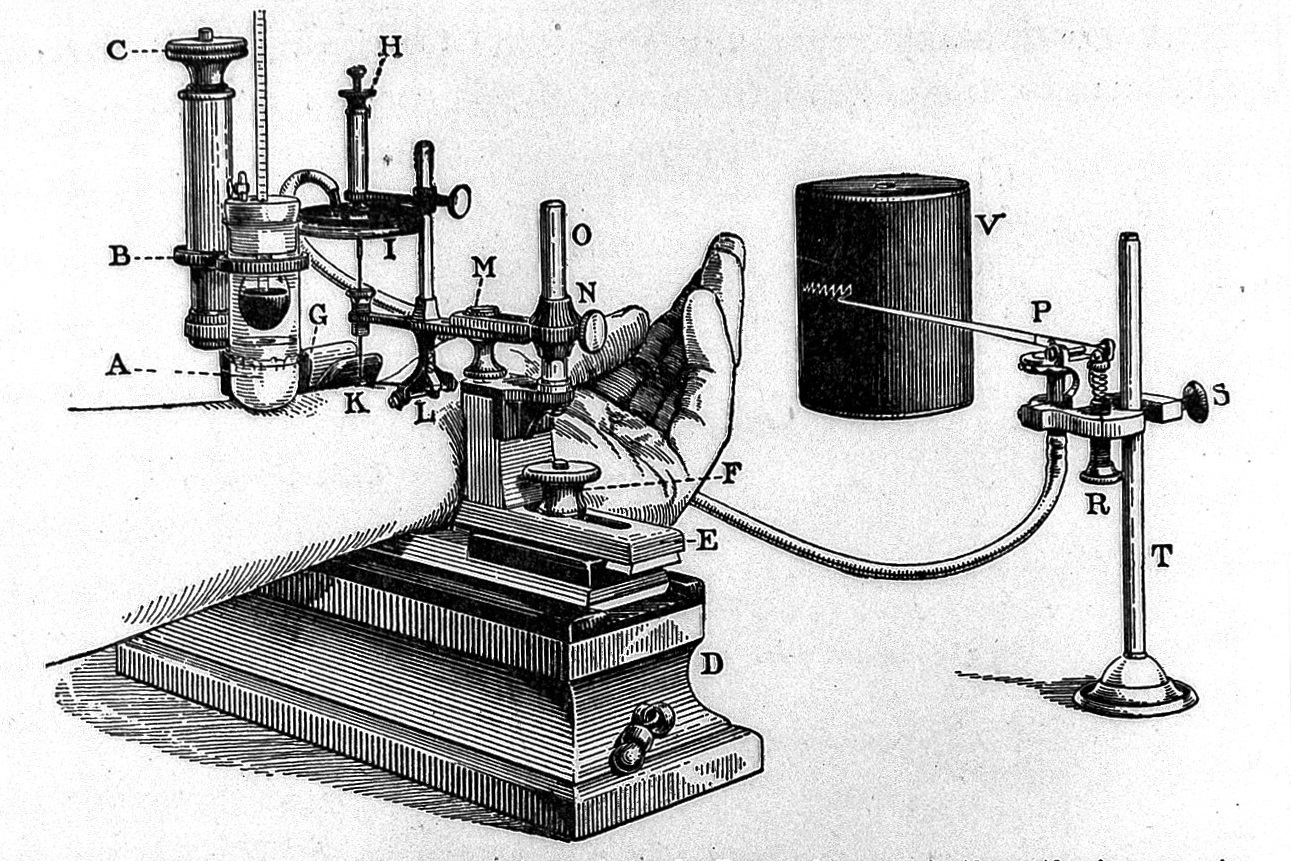
Basch's sphygmomanometer. Credit: Wellcome Collection
In 1896 Italian paediatrician Scipione Riva-Rocci (1863–1937) introduced his mercury sphygmomanometer, a piece of equipment that would look familiar to people today. The sphygmomanometer used an inflatable rubber cuff around the circumference of the patient’s arm to obstruct the blood flow of the brachial artery. This pressure measurement is known as systolic, and is the force at which your heart pumps blood around your body. This technique meant the brachial artery was compressed equally from all sides. This was an improvement on Von Basch’s technique which took the measurement from one place.

Riva-Rocci's mercury sphygmomanometer. Credit: Wood Library-Museum of Anesthesiology
Riva-Rocci’s method however did not measure the diastolic pressure (the resistance to the blood flow in the blood vessels). In 1897, the Hill and Barnard sphygmomanometer, named after its designers Dr Leonard Hill, a British physiologist, and Harold Barnard, a British surgeon, included a needle pressure gauge which was sensitive enough to record the diastolic pressure.

The Hill and Barnard sphygmomanometer. Credit: Science Museum Group
In 1901, Heinrich von Recklinghausen increased the size of the cuff used with Riva Rocci's equipment from 5cm to 12cm wide. This improved the accuracy of readings by reducing localised areas of high pressure build up.
In 1905, Russian surgeon Nicolai Korotkoff described the sounds heard through a stethoscope placed over the brachial artery during slow deflation of a Riva Rocci cuff. This became the most widely used method of blood pressure measurement.
Despite these early developments, measuring blood pressure during anaesthesia first took place in 1901. However, measuring blood pressure as a health check only became common practice from the 1920s.
After the introduction of cyclopropane in 1934 and curare for anaesthesia in 1942, which made deep general anaesthesia unnecessary, excessive bleeding became increasingly problematic in surgery. Significant blood loss was a great risk to the patient and could impede a surgeon’s work. This is where planned hypotension provided a solution. This technique was seen to be a means of controlling bleeding where otherwise it may be severe and difficult to control[1], or where even a small amount may adversely affect precision of exposure and the ultimate result, for example in thoracolumbar sympathectomy and certain plastic procedures.
In 1948 Harold Griffiths and John Gillies trialled a technique whereby they deliberately reduced a patient’s blood pressure to a point where it was un-recordable by the normal means of a cuff. The aim with reducing the patient's blood pressure to a level significantly below normal was to provide a near bloodless field of operation, which it did successfully.
Through induced hypotension, it was found that a patient could tolerate an arterial pressure of around 60mmHg for several hours without damage to the brain or other organs. A similar period of hypotension due to blood loss would however often prove fatal. Considering also that hypertension was the second-most common factor associated with postoperative morbidity in the 1950s[2], the benefits to the patient are apparent.
For the surgeon, the advantages of hypotension are clear; their work is made easier and can be done more quickly. These and other benefits, particularly the ability to maintain a constant blood volume, also benefit the patient as long as the hypotensive technique is competently controlled.
After the experiment, John Gillies noted that the technique of induced hypotension represented ‘physiological trespass’, as the normal safety margins were eroded. For example, decreased blood pressure will cause a decrease in blood flow if an artery is blocked by disease, meaning patients with arterial disease who were subject to this technique might suffer a stroke or coronary thrombosis.
By 1953, it became clear that the technique of induced hypotension had resulted in some deaths, and it was used more cautiously. It was reserved for operations likely to have significant blood loss (i.e. brain aneurysms), or where a large amount of tissue had to be removed (i.e. in cancer).
Controlled hypotension not only minimised blood loss for major surgeries, it provided a greater understanding of circulation. Through observing the effects of dilating the blood vessels by various means, such as changing the venous return to the heart by posture, increased lung pressure, or by modifying blood volume, new knowledge of the behaviour of the circulation was gained by anaesthetists which improved anaesthetic practice.
This greater understanding of the body system led to further improvements in the way the body could be controlled to improve patient safety. For example, in the early 1950s, induced hypothermia (decreasing the patient’s body temperature from 37 -30c) was found to half the brain’s oxygen consumption, which doubled the amount of time the body could be without blood flow, which improved cardiac and neurological surgeries.
Drugs which control hypertension were introduced during the 1940s. Pharmacology still manages a patient’s blood pressure. Vasodilating drugs are used when the patient develops significant hypertension during surgery or after cardiac operations. Perioperatvely, patients also benefit from being given antihypertensive drugs to reduce the risk of heart attack.
References
- Proceedings of the Royal Society of Medicine Vol.45, September 7, 1951, Physiological Trespass in Anaesthesia
- Measurement of Adult Blood Pressure