Your letters
Dear Editor
GlideScope Auto Power Off – a nasty surprise
We used a GlideScope (Verathon Inc., Bothell, WA, USA) for a difficult
tracheal intubation in a patient with severe burns to the head, neck
and chest. As a bougie was being inserted into the mouth, the
screen went blank, leading to a delay while the instrument restarted;
however the oxygen saturation remained > 96%.
Like many other instruments that have limited battery back up, the
GlideScope has an adjustable Auto Power Off function to conserve
screen and battery life, with a factory default of 30 min. In this case,
the ODP had turned the machine on (and plugged it into the mains
supply) considerably in advance while preparing the equipment for
anaesthetic induction. However, we did not realise the Auto Off was
set at 20 min (Figure 1), nor did we notice the imminent shut-down
message on the instrument screen (Figure 2).
We all know the old adage “Know thine enemy”. It is also important
to get to know your friends thoroughly.
Toby Ma
Anaesthetic Clinical Fellow
East Midlands Deanery
Figure 1. Screen showing Auto Power Off menu
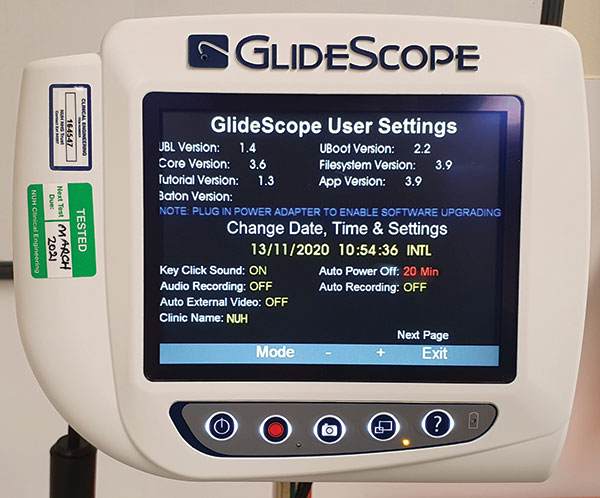
Figure 2. Warning screen before shut down

Congratulations to Toby Ma for winning
February's Letter of the Month prize.
Dear Editor
COVID-19 airway assessment: public masks = anaesthetists’ angst
I wish to highlight a hitherto unreported, but highly significant,
consequence of COVID-19 on the wellbeing of anaesthetists.
The recently mandated wearing of facemasks in enclosed public
spaces, in particular on public transport, has robbed us of a
favourite anaesthesia pastime - “How would I manage his/her
airway?” (insert random passer-by/ fellow passenger).

I strongly recommend anaesthetists affected by these new
government regulations seek immediate professional help from
their local anaesthesia coffee room support group. It is crucial to
acknowledge the effect this may be having on morale, and to
share any negative emotions with others, who may be experiencing
similar feelings of loss and emptiness!
Fortunately, there is still at least one pastime to keep us
anaesthetists happy - “What size cannula could I insert into
his/ her vein?”
Patrick Alexander Ward
Consultant Anaesthetist and Airway Lead
Chelsea & Westminster Hospital, London
Dear Editor
The COVID Novice
I have a confession; I am a senior anaesthetic trainee who has
never cared for a COVID patient. By a peculiar twist of fate, I have
‘dodged’ working during the biggest healthcare crisis for 100
years. I do have a healthy (and rather large) baby boy to show for it,
born two days into lockdown, while COVID guidelines pummelled
my WhatsApp inbox.
Soon, however, I will return to work. The world has changed. When
we leave the house, we check for our facemask as we do our keys
or phone, and to ‘Zoom’ is a verb. Lost in a shop’s inexplicably
complicated one-way system, I wonder how I will navigate the new
hospital landscape.
Fortunately, I am part of a supportive School of Anaesthesia, with
an excellent return-to-training programme. However, I cannot help
but think that there will be subtleties and nuances that cannot
be taught or simulated, and theatre etiquettes that have evolved
organically and are now embedded in hospital culture. All of these
will be alien to those who have watched the pandemic from the
side lines.
Returning to work has a new dimension. Not only do we need to
remember how to do the job we know, we need to learn to do a
job that we never did. So, if you see a COVID-novice, staring at a
cannula, wondering not only whether they can still put one in, but
also what attire they should don to do so, offer some pointers and
socially distanced reassurance. Also, if anyone can explain the oneway
system in my local WH Smith, that too would be appreciated!
Emma Jenkins
ST7 Anaesthetics
Southmead Hospital, Bristol
Dear Editor
With reference to the letter by Kler et al. on Page 30 of the
December issue of Anaesthesia News, ‘How many times can one
prone a patient with COVID-19 pneumonia?’:
‘Prone’ is an adjective. Can I also be ‘supined’?
I am iPadding this thought. Or should I be iPading it?
With respect
Robin Weller
Retired amateur editor
Sent from my iPad
PS In no way, I would emphasise, is this a criticism of the authors
of the letter in which this new verb appeared. I remain amazed
how the ICUs have managed throughout this dreadful year.
Makes me quite proud to be an Honorary Member of the
Association to which so many anaesthetists belong.
Editor's reply
Like Dr Weller, I don't like the tendency to change nouns or
adjectives into verbs, but I'm not going to get into an ipaddy
about it.
Prone/ proning/ proned is much easier for communication
purposes than 'turn/ turning / having turned the patient into the
prone position'. In support of its current use, Google Scholar
finds the terms 'proned' + 'covid' in > 17,000 places.
I am with King Canute on this one.
What do our readers think?