Your letters - December issue
Dear Editor
i-gel® Christmas tree
I would like to showcase the creative talents within our
ODP / Anaesthetic Nursing team. Lessley (pictured) is
from a family of artists, and her i-gel® ‘cradle’ Christmas
decorations have been in high demand in our
department.
A brief review of the literature (Googling ‘i-gel
Christmas tree’) reveals that she is not the only person
who has come up with this idea. However, owing to her
avoidance of all things social media, I can vouch that
Lessley came up with the concept independently.
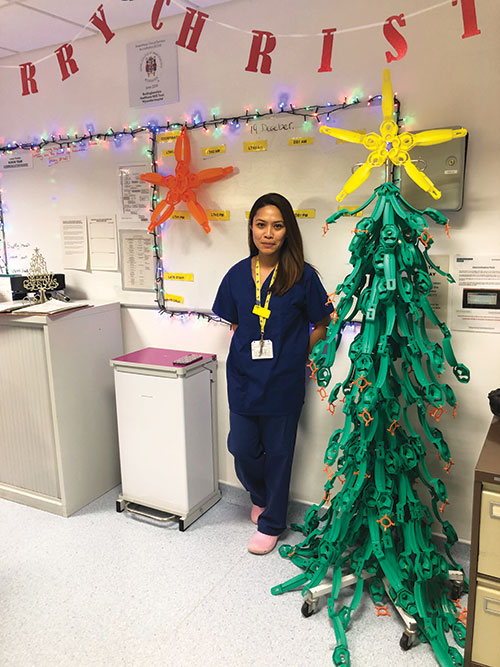
We all recognise the need to Reduce, Reuse, Recycle
as much as possible. Here is a great example of Repurposing
used packaging. We are also faced with the
daunting challenge of trying to improve well-being in
a system that is under more strain than ever before.
There is an unquantifiable additional benefit to the i-gel
Christmas tree in the smiles that it induces.
Carl Morris
Consultant Anaesthetist
Buckinghamshire Healthcare NHS Trust
Dear Editor
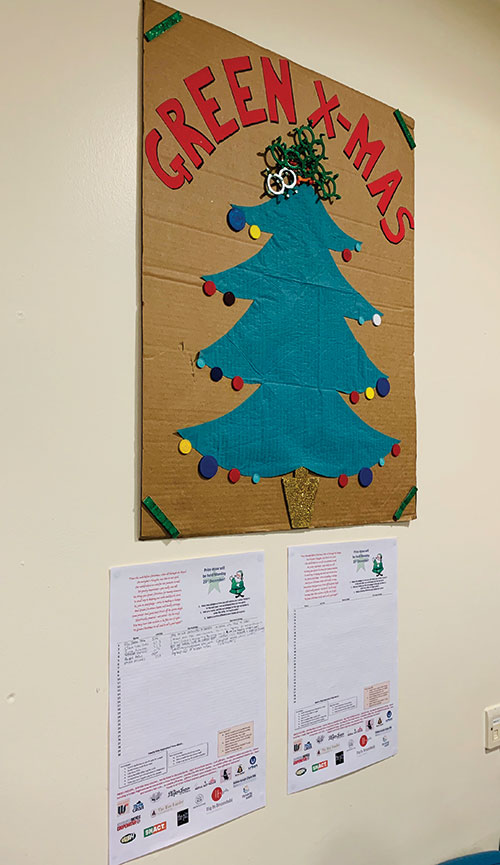
The Green Christmas Initiative
There has been a recent call to arms for anaesthetists to promote
environmental sustainability [1, 2]. We are implementing strategies to
decrease the carbon footprint in our hospital; however we have found
that awareness of, and passion for, the cause were low in some of our
staff. To address this, we ran a ‘Green Christmas initiative’ for two weeks
in December 2019. Posters were made from recycled materials, such as
plastic rings from face masks and cardboard boxes from theatre stores
(Figure 1), which were placed in theatre coffee rooms. Staff signed up to
sustainability pledges for work and home. Participants were entered into
a prize draw, with all prizes being supplied by our generous sponsors –
all affiliated with environmentally friendly produce. Over 100 staff made
pledges, such as ‘teaching TIVA to junior trainees’, ‘cycling to work’,
‘recycling syringe packaging’, and ‘being vegetarian for January’. Twentyeight
prizes were given out by our Green Christmas Santa, including bike
shop vouchers, reusable coffee cups, personalised theatre hats, exercise
classes and vegetarian meal boxes. The initiative was multidisciplinary,
being organised by staff from anaesthesia, recovery and pharmacy,
and advertised to all theatre staff. This has helped to emphasise that
sustainability is a matter for everyone’s concern. However, we found
that few surgeons participated, highlighting that this group should be
specifically targeted in future sustainability projects.
This was a fun and celebratory way to think about sustainability, in contrast
to the frequent pessimism encountered when approaching the subject.
We aim to repeat the Green Christmas initiative in 2020, and to maintain
the enthusiasm for sustainability that it has generated in our hospital. We
encourage other departments to consider similar initiatives in order to
increase awareness of the sustainability challenges that exist in theatres,
and to consider enacting small changes to make a big difference.
Figure 1. Green Christmas poster in the coffee room
Emma Claire Phillips
ST3 Anaesthesia
Andrew Grant
Consultant Anaesthetist
Lydia Howell
Recovery Nurse
Alifia Chakera
Lead Pharmacist
Royal Infirmary of Edinburgh
References
- Association of Anaesthetists. Long
term strategy, 2019. https://anaesthetists.
org/Portals/0/PDFs/About%20us/
Policies%20and%20processes/
Association%20of%20Anaesthetists%20
long%20term%20strategy%202019.
pdf?ver=2019-05-24-111746-190
(accessed 15/1/2020).
- Royal College of Anaesthetists.
Sustainability strategy 2019 – 2022,
2019. https://www.rcoa.ac.uk/
about-college/strategy-vision/
environment-sustainability/sustainabilitystrategy-
2019-2022 (accessed
15/1/2020).
Dear Editor
The i-gel® protective cradle is now recyclable - manufacturer’s response
Further to Dr Hickman’s letter in the June issue of Anaesthesia News
confirming that the protective cradle and cage pack of the Intersurgical i-gel®
supraglottic airway can be recycled [1], we would like to thank Dr Winkley for
highlighting in the August issue that she had found a company in the North-
East who recycle clean plastic waste from industry [2]. We note that a plastic
recycling trial for Northumbria NHS Trust is now in progress with this company,
recycling clean plastic waste from the hospital including the i-gel protective
cradles. This is positive news.
However, recognising that the healthcare sector is a large producer of plastic
waste, Dr Winkley also asked whether it is necessary to produce such waste in
the first place. In the case of the i-gel, we can confirm that the protective cradle
(adult sizes) and cage pack (paediatric sizes) ensure that the product remains
in the correct flexion prior to use, and are therefore essential for patient safety
and product performance. They also help to optimise gas circulation for
effective sterilisation, and act as a base for lubrication.
We can also confirm that Intersurgical are certified to international
environmental standard ISO 14001, and are committed to the protection of
the environment by minimising the environmental impacts of the company’s
products, activities and services, including the prevention of environmental
pollution and sustainable resource use. This process includes regular review of
existing products and packaging, and we will continue to investigate ways in
which we can reduce the packaging for our products, including the i-gel.
David Chapman
Airway Group Product Manager
Intersurgical Ltd
Wokingham
Twitter: @daveairways
References
- Hickman J. The i-gel® cradle is now recyclable. Anaesthesia News 2020; Issue 395: 42.
- Winkley E. The i-gel© cradle is now recyclable - a response. Anaesthesia News 2020; Issue 397: 31.
Dear Editor
COVID-19 airway assessment: unmasked
In this COVID-19 era, I would like to reinforce the
importance of continuing to undertake a thorough
airway assessment before commencing anaesthesia.
Face-to-face interactions with patients are likely
to be replaced with virtual consultations where
possible, adding a new dimension to airway
evaluation. The accuracy of remote assessment is
yet to be established, but is likely to benefit greatly
from a standardised approach, agreed locally by
departments, and undertaken by experienced staff.
Patients presenting on the day of surgery will now
routinely be wearing facemasks. After appropriate
screening questions and assessments, the patient
should be asked to remove their mask briefly to
enable a full airway evaluation from an appropriate
distance.
Airway assessment in the patient with respiratory
failure may be complicated by non-invasive positive
pressure ventilation masks or hoods. Ideally, an
advance airway assessment should be undertaken
(and documented) before commencing noninvasive
ventilation, in order to plan a future airway
strategy. Should tracheal intubation become
necessary, an immediate airway assessment by the
designated primary intubator is still recommended,
informed by the initial evaluation. In this situation,
many of the standard bedside tests are still possible,
even with the mask or hood remaining in situ.
Patrick Alexander Ward
Consultant Anaesthetist
Chelsea & Westminster Hospital, London
Dear Editor
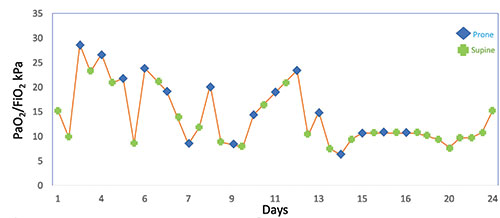
How many times can one prone a patient with COVID-19 pneumonia?
While tackling COVID-19, many of us are pushing treatment options to the extreme. These
patients may develop respiratory failure similar to that seen in ARDS [1]. In severe ARDS, it
has been recognised that early prolonged proning is linked with improved 28- and 90-day
mortality, although the maximum duration of proning has not been established [2].
Two subtypes have been identified in the critically ill patient with COVID-19, type 1 (non-
ARDS) and type 2 (ARDS) [3]. Patients with type 2 have a better response to proning. Lung
compliance is low and elastance high, with large portions of non-aerated lung tissue,
therefore proning improves recruitment of this lung tissue [3]. Most prone ventilation
practices involve 16 h in the prone position with 2- 3 hourly head turns, and 8 h in the supine
position [4]. Figure 1 shows the effects of proning on the PaO2/FiO2 ratio of a patient who
was proned 16 times over a 14-day period, with good effect despite clear variability in
response. This patient survived to discharge.
Proning for a prolonged time often leads to complications, including pressure damage
at pressure points and from tube ties. Significant oedema to lips, tongue and eyes have
also been recorded. The need for head turns while proned poses a risk of tracheal tube
malposition and ventilator disconnection. Two of our patients who were proned for a
prolonged period of time developed brachial plexus injuries, which were confirmed on
nerve conduction studies [5].
The number of times a patient can be proned is determined by the response to proning
and appropriate patient selection. Perseverance may be the key to success.
Prabhjoyt Kler
Specialty Registrar, Intensive Care Medicine/ Anaesthesia
Matthew Byrne
Speciality Registrar, Anaesthesia
Timothy Scott
Nageswar Bandla
Consultant Intensivists/ Anaesthetists
University Hospital North Midlands, Stoke-on-Trent
Congratulations to Prabhjoyt Kler for winning December's letter of the month prize
References
- Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: a review. Clinical Immunology 2020; 215: 108427.
- Guérin C, Reignier J, Richard J-C, et al. Prone positioning in severe acute respiratory distress syndrome. New England
Journal of Medicine 2013; 368: 2159-68.
- Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not? Critical Care 2020; 24: 154.
- Faculty of Intensive Care Medicine/ Intensive Care Society. Guidance for: prone positioning in adult critical care, 2019.
https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf (accessed 11/9/2020).
- Malik GR, Wolfe AR, Soriano R, et al. Injury prone: peripheral nerve injures associated with prone positioning for
COVID-19-related acute respiratory distress syndrome. British Journal of Anaesthesia 2020 in press.
Dear Editor
Tea trolley model of training
We would like to highlight how we have
used our anaesthetic rooms, unused for
clinical purposes during the COVID-19
pandemic, for training.
We have found that our ability to
provide simulation training has
decreased because of: difficulty in
getting staff together to train due to
clinical pressures; requirements for
social distancing; and the need for a
COVID-secure environment where staff
providing care for patients on the ‘green
pathway’ remain separate from those on
the ‘amber pathway’.
To address this we have adopted the
‘Tea trolley’ model of training [1]. A
trolley containing equipment for a
10 min simulation is brought into the
anaesthetic room. The anaesthetist and
ODP working in theatre are relieved
by members of the training team, doff
their PPE, and perform the simulation
facilitated by other members of the
team. They are then given a drink and
cake during the debrief.
Utilising our anaesthetic rooms provides
us with a private area for training that
does not interfere with clinical work in
the theatres. Working our way along
the corridor, starting in ‘green’ and
moving on to ‘amber’, prevents crosscontamination
and maintains the COVIDsecure
environment.
Our first session on management of
the difficult airway and front-of-neck
access was well received. We intend
to continue this form of training as the
pandemic progresses.
Su-Mei Tham
Clinical Fellow
Victoria Wroe
Hannah Wrigley
Consultant Anaesthetists
Warrington and Halton Hospitals
References
- O'Farrell G, McDonald M, Kelly FE. 'Tea trolley'
difficult airway training. Anaesthesia 2015;
70: 104.