Single use airway devices:
Harms and solutions
Annually the NHS in England procures and disposes of 32.3 million (m) airway devices
purchased for £56.9m. These devices are used for general anaesthesia and includes 18m
supraglottic devices (SGDs), 5.3m endotracheal tubes (ETTs), 4.4m tracheostomy tubes and
2.9m laryngoscope blades. Here we discuss the origins of single use airway devices and
suggest routes toward responsible and sustainable alternatives.
Most airway devices are made of plastic. Plastic became widely available in the 1960s and as a material offers many advantages:
it can be made flexible or rigid, is airtight, waterproof and cheap. However plastic manufacture is characterised by the extraction,
refinement, combustion and dispersal of organic hydrocarbons (oil) and their polymers, with the addition of plasticising chemicals
(typically phthalates or esteric aromatic compounds) to soften the finished product. The manufacturing process takes refined oil
as both substrate and energy source, emitting pollution in the form of carbon dioxide and particulate matter. In the UK airway
devices are typically used once and disposed of in energy and carbon-intensive waste streams (typically incineration), emitting
further carbon dioxide.
Most disposable laryngoscope blades are manufactured from steel, in northern Pakistan, and aligned with the principle of cost
reduction, this includes the use of sweatshops, child labour, and welding equipment with limited personal protection [1].

Single use and the airway
Association of Anaesthetists current guidance states that
laryngoscope blades and handles, ETTs, SGDs and oro/
nasopharyngeal airways must be high-level disinfected or
sterilised as these devices may become contaminated with
blood, occasionally breaching a mucosal barrier [2]. The
guidelines encourage the procurement of single use devices
(SUDs).
A significant factor in the historical move to single use
laryngoscope blades was the identification of variant CreutzfeldJakob disease (vCJD) caused by a prion protein that can reside
in oropharyngeal lymphatic tissues of those with end-stage
vCJD. Continued use of SUDs has been perpetuated by the
fact that the single use approach eliminates other infection
risk, including the transmission of respiratory pathogens. SUDs
also offer convenience and alleged cost savings compared to
reusable devices, especially where the infrastructure to enable
devices to be reused is lacking (many hospitals lost sterile
services capacity during the vCJD scare).
At present, most airway devices in the UK are single use. A
survey of hospitals in the UK showed that 95% (21/22) used
single use laryngoscope blades [3]. Most other airway devices
are also single use, although reusable SGDs, laryngoscopes
and videolaryngoscopes are commercially available. The notion
of single use has even extended to flexible bronchoscopes,
described as a possibly cost-effective solution: apparently
through avoiding costs of repair, reprocessing, maintenance and
risk of litigation.
Whilst we agree that it would be unacceptable to compromise
safety in favour of an improved environmental profile, we need
to re-appraise the belief that single use airway devices are best.
Myth 1: Re-use is an infection risk
A recent review found a lack of evidence to support the
argument that SUDs reduce the incidence of nosocomial
infections [4]. In the 1970’s there were a few cases of
transmission of vCJD between patients linked to neurosurgical
equipment and predated sterilisation, but vCJD has never
knowingly been transmitted by airway devices. Testing of over
62,000 tonsil specimens in the UK has never found evidence
of prion protein [5], and in England and Wales, tonsillectomy
has been performed using reusable instruments and steam
sterilisation since 2001 [6]. It seems nonsensical to not apply the
same approach to airway devices. The UK National Prion Clinic
agrees, and they advise: ‘For patients who are not suspected
to have prion diseases we don't think there is a requirement for
single use anaesthetics equipment’ [7].
Nevertheless, contaminated laryngoscope blades have been
linked to the deaths of critically ill patients [8] and a lack of
standardised reprocessing procedures was previously a
recognised concern [9, 10]. This does not mean that we need
SUDs, rather it means that we should explore reliable methods
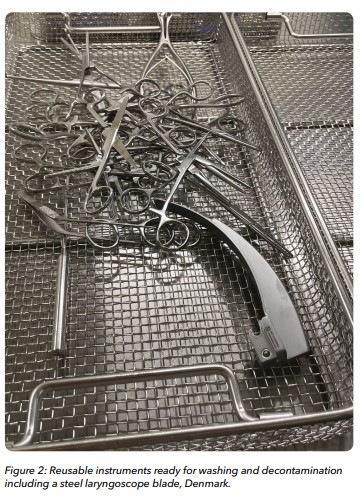
for decontamination and sterilisation. In other settings, steam
sterilisation and the reuse of laryngoscope blades are the norm.
Contrary to myth, disposable laryngoscopes carry a greater
bioburden when compared with reusable sterilised devices.
Disposable laryngoscopes are disinfected rather than sterilised,
with thresholds of acceptable bioburden set by manufacturers
in accordance with international standards (ISO 11737-1).
Importantly however there has been no study comparing
infection rates between reusable and disposable laryngoscopes.
Airway interventions are inherently non-sterile procedures
and involve an anaesthetist in non-decontaminated attire
and gloves; the source of infection may be independent of
laryngoscope type.
Myth 2: Single use is better for the environment
Multiple studies show the general principle that reuse of
medical equipment is better for the planet, the same is true
for airway devices. Single use plastic laryngoscope handles
represent up to 18 times the carbon footprint compared to
reusable steel [11]. Similarly, 40 single use SGDs have a lifecycle
carbon footprint of 11.3 KgCO2e, 1.5 times greater than a
reusable device used and decontaminated 40 times [12].
Myth 3: Single use is financially cheaper
In one study from Australia, the cost of using 4490 disposable
laryngoscope blades each year was estimated to cost £6000
more than using reusable equivalents [13]. A UK analysis
suggested reusable laryngoscope blades cost almost half that
of single use [14], and by extrapolation, this would save the NHS
£4.9m per annum.
The future
In summary, SUDs are costly for the public purse, the
environment and global society. Reusable alternatives to some
devices exist, with tried and tested reprocessing techniques to
ensure safety and reliability. However, there is a need for further
industrial and clinical research into reusable device design and
novel and reliable decontamination techniques. Alongside this,
we must advocate for national and international policy maturity,
away from over-zealous precaution and towards an evidencebased assessment of risk, that also considers planetary and
societal harm from the single use culture.
James Dalton
Anaesthesia Sustainability Fellow, University Hospitals Sussex
NHS Foundation Trust
Richard Newton
Consultant Anaesthetist & Environmental Anaesthesia Lead,
University Hospitals Sussex NHS Foundation Trust
Mahmood Bhutta
Chair of Ear, Nose & Throat Surgery & Professor of Sustainable
Healthcare, Brighton and Sussex Medical School
References
1. Bhutta M; Santhakumar A. Labour rights and violation in the manufacture of healthcare goods. ENT & Audiology News. 2015; 24: 1
2. Association of Anaesthetists. Infection Prevention and Control Guideline, 2020. URL: https://anaesthetists.org/Home/Resourcespublications/Guidelines/Infection-prevention-and-control-2020 (Accessed 06.11.2023)
3. Ghandi J; Campbell G. Unpublished data. Reusable vs single use infection control policy. Association of Anaesthetists Survey. 2022
4. Reynier T; Berahou M; Albaladejo P; Beloeil H. Moving towards green anaesthesia: are patient safety and environmentally friendly practices compatible? A focus on single-use devices. Anaesthesia, Critical Care & Pain Medicine. 2021; 40: 100907
5. Clewley J P; Kelly C M; Andrew N; et al. Prevalence of disease related prion protein in anonymous tonsil specimens in Britain: cross sectional opportunistic survey. British Medical Journal. 2009; 338: b1442
6. Clarke M B; Forster P; Cook T M. Airway management for tonsillectomy: a national survey of UK practice. British Journal of Anaesthesia. 2009; 99: 425–428
7. UK National Prion Clinic (University College London) email to J Gandhi (Association of Anaesthetists) 07 April 2022
8. Jones B L; Gorman L J; Simpson J et al. An outbreak of Serratia marcescens in two neonatal intensive care units. Journal of Hospital Infection. 2000; 46: 314-319
9. Negri de Sousa A C, Levy C E, Freitas M I. Laryngoscope blades and handles as sources of cross-infection: an integrative review. Journal of Hospital Infection. 2013; 83: 269-275
10. Machan M D. Infection control practices of laryngoscope blades: a review of the literature. American Association of Nurse Anesthesiology. 2012; 80: 274-278
11. Sherman J D; Raibley 4th L A; Eckelman M J. Lifecycle assessment and costing methods for device procurement: comparing reusable and single-use disposable laryngoscopes. Anaesthesia & Analgesia. 2018; 127: 434-443.
12. Eckelman M; Mosher M; Gonzalez A; Sherman J. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anaesthesia & Analgesia. 2012; 114: 1067–1072.
13. McGain F; Story D; Lim T; McAlister S. Financial and environmental costs of reusable and single-use anaesthetic equipment. British Journal of Anaesthesia. 2017; 118: 862-869
14. Unity Insights & Kent Surrey and Sussex Academic Health Sciences Network. Carbon savings laryngeal blades and suture kits, 2022.
15. URL: https://unityinsights.co.uk/our-insights/carbonsavings/#:~:text=On%20the%20carbon%20emissions%20 front,52%25%20and%2090%25%20respectively (Accessed 06.11.2023)