#KnockItOut – tackling workplace bullying, harassment and undermining
What is bullying?
“You must be aware of how your behaviour may influence others
within and outside the team”
states the GMC's good medical
practice document, our professional code of conduct [1]. How
we behave whilst at work affects those around us, but this may
be easy to forget in the heat of the moment. Examples of
unprofessional behaviours such as rudeness, incivility, belittling
and humiliation are frequently found in most hospitals.
Medicine
has a traditional, hierarchical culture, and this may lead to those
in positions of power misusing their status and/ or shielding
such perpetrators of bad behaviour from censure. When an
individual uses their positional power in a way that leaves the
victim(s) feeling hurt, angry or powerless, this is bullying [2].
Social bullying involves unacceptable jokes related to protected
characteristics (e.g. gender, race), public insults, practical jokes,
slander and exploitation [3]. The line between ‘banter’ and
bullying can be a fine one, and it is the perception of the victim
that defines bullying, not the intention of the perpetrator [2].
Does bullying and harassment occur in the NHS?
One fifth of NHS staff reported experiencing bullying and
harassment by colleagues in last year’s NHS staff survey.
Unrealistic time pressures, staffing shortages and stress were
identified as factors contributing to bullying behaviour [4]. This
survey looked at all NHS staff, but is this specifically a problem
amongst medical staff?
The 2017 BMA survey of 7887 doctors found similar results [5, 6].
Twenty percent reported being subjected to workplace bullying
or harassment, and 39% identified that bullying, harassment
or undermining behaviour had occurred where they worked.
This suggests that being a bystander to an incident of bullying
or harassment is common amongst doctors. The survey found
bullying affects consultants and trainees fairly equally, with
disabled, LGBT and BAME doctors reporting higher levels.
When asked,
“Why do you think there is or may be a problem
with bullying in the NHS?”
familiar themes included staff under
pressure, difficulty in challenging poor behaviours from seniors,
and a lack of management commitment to tackling bullying.
A
lack of clarity as to what is acceptable behaviour, and a lack of
clear reporting procedures, were also felt to contribute.
More recently the incidence of bullying amongst non-training grade doctors has been highlighted, with 30% of SAS doctors
and 23% of locally-employed doctors reporting they had been
bullied, undermined or harassed at work in the last year [7].
Rudeness, incivility, belittling and humiliation were the most
common types of undermining behaviour reported. When
bullying relating to protected characteristics was reported, race
was the most commonly cited factor.
Do we have a problem with bullying and unprofessional behaviours in anaesthesia?
Specialty specific data is surprisingly difficult to come by. The
most recent GMC national training survey that had a specialty
breakdown of bullying and harassment was in 2017 [8], reporting
that 4.6% of anaesthesia trainees described experiencing, or
witnessing, bullying and harassment at work. This is a lower
incidence than that reported by our surgical trainee colleagues,
where 8% of surgical respondents and 11.2% of obstetrics
and gynaecology respondents reported being victims of, or
witnessing, bullying and harassment. While it may not be an
overwhelming problem in anaesthesia, it is plausible that we
are frequent observers of bullying and undermining in other
staff groups through our multi-disciplinary working environment
in theatres and on the labour ward. We are working with the
psychology research team at Northumbria University on a
project to study trainee anaesthetists’ experiences of witnessing
workplace bullying to investigate this further.
What are the effects of bullying in healthcare?
Research has demonstrated that merely witnessing incivility and
unprofessional behaviours can cause a performance decrease
of 20%, and worryingly this incivility can spread, with witnesses
being less helpful to others even if they are unconnected to the
event [9]. Exposure to bullying, either as a victim or bystander,
is also associated with negative job-related and health- and
wellbeing-related outcomes. There is an increase in mental and
physical health problems, symptoms of PTSD, burnout, increased
intention to leave the organisation, reduced job satisfaction,
and organisational commitment. Workplace bullying is also
associated with employee absenteeism, negative performance
self-perception, and poor sleep [10].
There are serious effects on patients too; in NHS organisations
where staff surveys report bullying, patients are less likely to
report being treated with dignity and respect [11]. There is a
strong association between bullying and the occurrence of
adverse events and compromised patient safety [12]. Indeed,
in his public inquiry into the failings at Mid-Staffordshire, Robert
Francis QC wrote;
“The common culture of caring requires a
displacement of a culture of fear with a culture of openness,
honesty and transparency, where the only fear is the failure to
uphold the fundamental standards and the caring culture”
[13].
Going beyond the individual health and wellbeing, the financial
cost of bullying is huge. These can be measured in terms of
sickness absence, employee turnover, diminished productivity,
sickness presenteeism, compensation, litigation and industrial
relations. A conservative estimate of the cost of bullying to the
NHS is £2.28 billion per year [14].

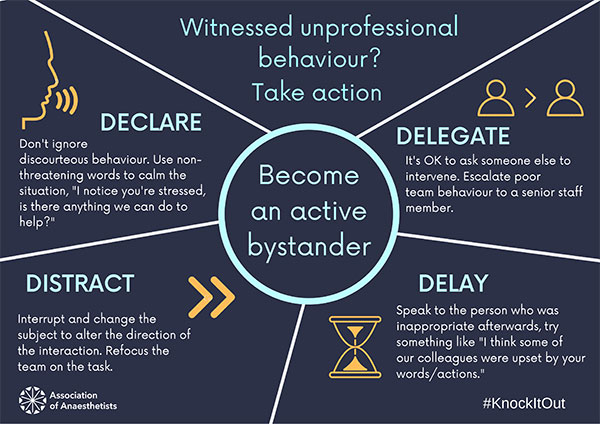
#KnockItOut
Through our #KnockItOut campaign, we want to change our
workplace culture to one that is free from bullying, harassment
and undermining behaviours. Whilst we endeavour to create
a compassionate culture, we need all our staff members to
be able to respond in constructive ways when they witness
unprofessional behaviour. We want to give them the tools to
confidently and successfully challenge these behaviours when
they see them. The active bystander approach has been used
in several anti-bullying and anti-sexual harassment campaigns
[15] – see Figure 1 for our version. Providing bystanders to an
incident with a framework to intervene safely is an important part
of changing the culture around bullying.
Being witness to a bullying incident can be frightening or
unsettling. There are times when reacting immediately may
involve being dragged into an argument, or cause further
unproductive behaviours. Taking a brief pause, recognising the
situation, responding constructively, and aiming for a measured
approach can help defuse the incident. We recognise that ‘one
size does not fit all’ in difficult situations, and aim to provide a
range of options to enable staff to intervene where appropriate.
We also recognise that one’s place in the organisational
hierarchy may alter how able one feels to challenge poor
behaviours; a junior staff member may well feel more able to
delegate to a trusted senior colleague in, or after, the moment.
The environments that we work in are increasingly stressful
places, making negative and unprofessional behaviours more
likely. Sometimes
declaring that you are aware of the situation, "I
notice you are a bit stressed, what can we do to help?",
will allow
the person under stress to ask for quiet, or perhaps assistance.
An indirect intervention by
distraction can be useful to change
the focus of the interaction, and to refocus on the task at hand.
Finally, the situation may not be suitable to be addressed in
the moment; in certain circumstances a
delay may be required.
Once the stressful situation has settled, speak to the person
who was inappropriate, stick to the facts as they happened, and
highlight how their words or actions were perceived by others.
In addition to providing intervention strategies, we want to
encourage a ‘SAFER’ space at work, where kindness and civility
are paramount, and staff work together towards a shared goal.
This can include engaging the team in a verbal run through of
likely stressful points in the day and how best to respond
“When
we get to the anastomosis can we turn the music off and have
quiet in theatre, please”
or “I’m expecting a challenging airway,
so can we not be interrupted during the intubation process,
please”
(Figure 2).
The Association of Anaesthetists is a member of the NHS
anti-bullying alliance, and by working together with the other
organisations involved we want to tackle the cultural and
systemic issues that contribute to bullying. It is time for us to
demonstrate as a profession that we are committed to change
and we will not tolerate unprofessional behaviour: it is time for
anaesthesia to #KnockItOut.
Roopa McCrossan
Association of Anaesthetists Trainee Committee
Locum Consultant in Anaesthesia, Freeman Hospital; Newcastle
Karen Stacey
Elected member, Association of Anaesthetists Trainee Committee
Locum Consultant Anaesthetist, Imperial College Healthcare NHS
Trust
Twitter: @RooMcCrossan; @karenstacey82