Supporting the shielded - results from a national survey of shielding doctors
In spring, NHS staff responded to the looming COVID-19 pandemic with an impressive level of strategic planning. As operating theatres closed and ICU beds were created, anaesthetists and intensivists faced new challenges on the ‘frontline’. However, a small and unknown number of these doctors were issued with stark instructions from the government to shield themselves from the crisis. Facing an unexpected disruption to careers and training, shielding doctors found themselves confined to their homes. This disconnection from the frontline created significant practical and psychological challenges.
Shielding advice was issued to those at highest risk of severe illness from COVID-19. The ‘extremely clinically vulnerable’ are those who have a specific set of conditions [1]. These include: solid organ transplant recipients; certain cancers; severe respiratory conditions; people with rare diseases at risk of infection; those on certain immunosuppressive therapies; and pregnant women with heart conditions. Shielding instructions are stringent and in place for months. Some doctors are shielding ‘by proxy’, to protect another adult or child within their own household.
In March 2020, a group of shielding anaesthetists formed a virtual support network to engage in discussions regarding employment practices, wellbeing, and other challenges. Their concerns have been highlighted in recent correspondence in Anaesthesia journal [2].
The issues raised within this group led to the development of a national survey of shielding doctors to assess the problem. An electronic survey containing 15 questions on professional and personal issues was created using Google Forms®, and was shared on social media between 20 May and 2 June. This article provides a summary of the answers - further information is available from the authors at [email protected].
A total of 116 doctors from 21 specialities responded, of whom 55 (47%) were anaesthetists or intensivists. Respondents included 55 (47%) consultants, 56 (48%) trainees, and 5 (4%) specialty doctors or associate specialists. Gender, age and ethnic minority were not requested. Sixty (52%) respondents were following the generic government advice, while others were following advice from their Occupational Health Department or a local risk assessment. One hundred and six (91%) respondents were shielding because of their own health issues, the others because of a family or household member. Immunosuppression and respiratory conditions were the most common medical reasons for shielding. Sixteen (14%) were pregnant.
Shielding affects individuals in different ways, but a common theme is the immediate switch from practising doctors to ‘extremely vulnerable’ members of society. Reported feelings about shielding include: guilt at not being able to help the NHS 103 (89%); frustration 80 (69%); anxiety 65 (56%); loneliness 52 (45%); and relief 40 (35%).
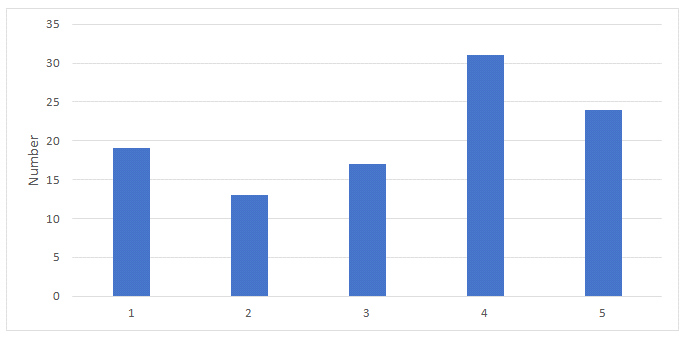
Responses to the support provided by employers and educational bodies (e.g. Health Education England) for shielding, and support provided by employers for remote working, are shown in Tables 1-3. Ninety-two (79%) of respondents reported working from home in clinical or supportive roles, such as education and management.
Sixty-one (73%) have changed their behaviour as a coping response. Some mentioned increased alcohol consumption, excessive focus on cleaning, or methods to keep themselves safe.
The impact on career and family was significant; the most common concern expressed across two questions was delayed progression through training (28 responses, 33%), and impact on career (28 responses, 30%). Twenty (22%) respondents reported uncertainty about the future.
When asked about returning to work, 32 (34%) were keen to get back but 49 (52%) respondents mentioned a high level of anxiety. Some reported feeling apprehensive and unprepared as they have been out of clinical practice, or worried that they will not fit into their department. A few stated that they have no plans to return to work until they feel safe or there is a vaccine. Some worry about the lack of strict adherence to social distancing among NHS staff. Knowing that their colleagues are aware of their health problems has made some feel ashamed and apprehensive.
Shielding ends on different dates for each UK nation (England 1 August; Scotland 31 July; Wales 16 August). There is a need to address these issues urgently. While return-to-work worry is not specific for medical professionals, the increased workplace infection risk compared with non-medical professions will make the process more daunting and the decisions more complex. An individualised approach, based on a robust risk assessment tool that links clinical vulnerability to workplace risk, will be the best way forward [3-7]. The SuppoRTT system [3], already set up by HEE for returnees from maternity and sick leave, could be modified effectively for trainees returning from COVID-19 shielding. Our survey demonstrates that long term planning, proactive discussions, and a flexible approach to training will be key to supporting shielding doctors.
The survey findings have raised some serious concerns about the mental health, wellbeing and experiences of shielding doctors. To date there has been minimal official guidance from national bodies, Royal Colleges, Deaneries or departments [9, 10]. Some of those shielding feel that they have been ‘forgotten’ and left in isolation, with no plan on how to return to work safely. As the pandemic threatens further waves, they also have concerns about the longer term.
It is now time for shielding doctors to be supported proactively with their careers and overall wellbeing. This might include, but is not limited to: opportunities for remote training and development; mentor allocation; comprehensive risk assessment; and supported return to work and training. Returning to work will require coordinated planning and agreement from national bodies, local departments, employers and the returnee.
Grace Swann
Foundation Year 1 doctor, Severn Deanery
Sethina Watson
Anaesthetic Registrar, Severn Deanery
Achuthan Sajayan
Consultant Anaesthetist, University Hospitals Birmingham
Twitter: @Grace_Swann; @morefluids; @Sajay70
References
- Public Heath England. Guidance on shielding and protecting people who are clinically extremely vulnerable from COVID-19, 23 June 2020. https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 (accessed 24/6/20).
- Iliff HA, Simpson KA, Tomlinson CR, Webb CM. ‘Shielded’ anaesthetists and intensivists during the COVID‐19 pandemic. Anaesthesia 2020; online version doi:10.1111/anae.15153.
- Health Education England. Supported return to training 2020. https://www.hee.nhs.uk/sites/default/files/documents/Supported%20Return%20to%20Training.pdf (accessed 24/06/2020).
- CIPD. COVID-19: returning to the workplace, 11 June 2020. https://www.cipd.co.uk/knowledge/fundamentals/emp-law/employees/workplace-guide-returning-after-coronavirus (accessed 24/06/2020).
- Association of Local Authority Medical Advisors. Covid-19 medical risk assessment, 23 June 2020. (ALAMA) https://alama.org.uk/covid-19-medical-risk-assessment/ (accessed 24/06/2020).
- medRxiv. Jankowski J, Davies A, English P, et al. Risk stratification tool for healthcare workers during the CoViD-19 pandemic; using published data on demographics, co-morbid disease and clinical domain in order to assign biological risk. medRxiv 2020.05.05.20091967; doi: https://doi.org/10.1101/2020.05.05.20091967 (accessed 24/06/2020).
- Welsh Government. COVID-19 workforce risk assessment tool, 18 June 2020. https://gov.wales/covid-19-workforce-risk-assessment-tool (accessed 24/06/2020).
- Faculty of Occupational Medicine. COVID-19 update: risk reduction framework for NHS staff at risk of COVID-19 infection, 12 May 2020. https://www.fom.ac.uk/wp-content/uploads/Risk-Reduction-Framework-for-NHS-staff-at-risk-of-COVID-19-infection-12-05-20.pdf (accessed 24/06/2020).
- Association of Anaesthetists. Guidelines. Vital signs in anaesthesia, April 2020. https://anaesthetists.org/Portals/0/PDFs/Guidelines%20PDFs/Vital_Signs_in_Anaesthesia2020.pdf?ver=2020-03-31-170128-410 (accessed 24/06/2020).
- British Medical Association. COVID-19: doctors isolating and those in vulnerable groups, 20 May 2020. https://www.bma.org.uk/advice-and-support/covid-19/your-health/covid-19-doctors-isolating-and-those-in-vulnerable-groups (accessed 24/06/2020).
Table 1. Support from employer (1 - none, 5 - excellent)
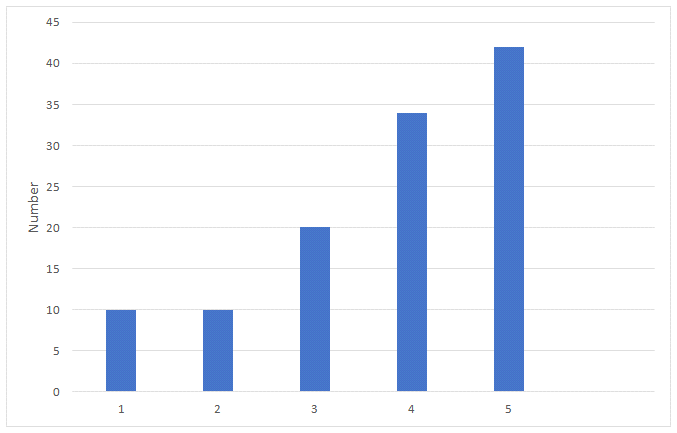
Table 2. Support for trainees from national educational bodies (1 - none, 5 - excellent)
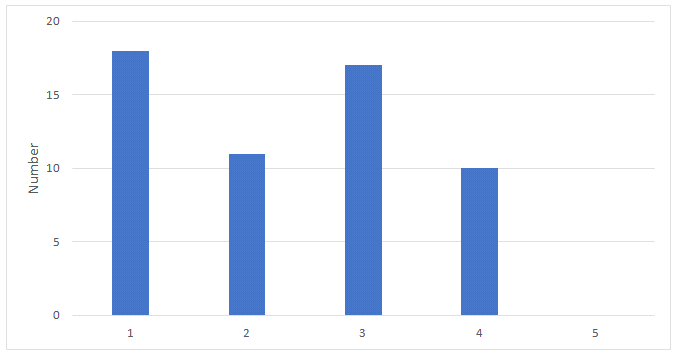
Table 3. Support from employer for working from home (1 - none, 5 - excellent)