ICU surge capacity in a busy London district general hospital during the COVID-19 pandemic
Northwick Park Hospital in North West London has been one of the hospitals hit hardest by the COVID-19 pandemic in the UK. Having one of the busiest emergency departments in London, and a tertiary infectious diseases service, we were designated as an additional high consequence infectious disease ICU [1]. On 3 March 2020 our ICU, with a baseline capacity of 22 beds, received the first patient with COVID-19, followed by a very rapid increase in admissions of patients who had undergone intubation and ventilation (Figure 1), peaking at 12 per day. On 12 March, the UK government moved from the ‘containment’ to the ‘delay’ phase of the pandemic management plan. During this transitional phase, we became one of the busiest hospitals in the UK with COVID-19 ICU admissions, reaching this at an earlier stage than others and with a greater mismatch between baseline-funded ICU beds and surge capacity beds, requiring a proportionately much greater and more rapid expansion. We write to offer some insights from the frontline about our management of hospital surge capacity.
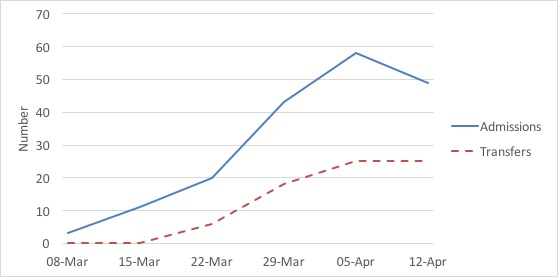
Figure 1. COVID-19 weekly admissions into (solid line) and transfers out of (dashed line) ICU.
The UK has far fewer ICU beds at approximately 6.6 per 100,000 population compared with the European average of 11.5 per 100,000 population [2]. In order to cope with the surge of COVID-19 cases into our hospital, we reorganised space, staffing, equipment and training to ensure a rapid upscale response to the crisis [3, 4]. Because of the rapidity of increase of infections, this response took place over a very compressed timescale and either pre-dated, or was contemporaneous with, national and London-wide surge planning [5].
Space: a rapid assessment was undertaken of all areas potentially able to provide a critical care environment, taking into account oxygen, power, isolation and sightlines. Our ICU beds expanded sequentially into: a 15-bed negative pressure isolation ward; operating theatres; post-surgical recovery; post-anaesthetic care unit; and medical wards. Within two weeks of admitting our first COVID-19 patient the ICU beds had doubled, and within four weeks had increased to 52 beds (236% of baseline) to meet the peak of the pandemic. Although every unit in the UK was expected to prepare for this level of proportional expansion, very few have had to put the plan into operation. Without a very effective regional mutual aid response from the North West London Critical Care Network, the forced expansion would have been much greater and exceeded the boundaries of temporary safe practice. In addition, an active acute respiratory High Dependency Unit expanded from six to 22 CPAP-capable beds over a short timescale, as clinical practice changed from early intubation to pre-emptive trial of CPAP and conscious proning. All non-urgent surgical procedures were cancelled to create capacity in advance of the date that this was introduced nationally.
Staffing: an early migration of ICU to a negative-pressure all-sideroom environment with a clean corridor was initially consistent with the national containment phase, but rapidly proved incompatible with flexed staffing ratios as the UK moved to the delay phase, resulting in early abandonment of this model and a move to cohorted working across several partially open units. Our highly experienced critical care nurses increased ICU nurse:patient ratios up to 1:4, with ward or operating theatre nurses working under supervision. Junior doctors from other specialties were redeployed to ICU, increasing the resident quota from 16 to 80 in less than three weeks. Intensive care and anaesthetic consultants moved to resident 12-hour shift working patterns, and worked together as a critical care team. Dedicated anaesthetic-led intubation and proning teams were created to meet demand.
Equipment: in order to increase the number of ventilators, early use was made of anaesthetic machines in ICU, supported by flexible working of operating department practitioners to provide technical support. With limited number of syringe pumps, we adapted infusions, including mixing propofol with fentanyl in the same syringe, and our pharmacy team worked to guarantee adequate stock of essential drugs or suitable alternatives.
Training: all staff were trained early to use PPE and undergo simulation scenarios. Cross-skilled nursing and medical staff from other specialties underwent a rapid critical care induction process that included lectures and practical-based skills training. The remarkable scaling up of material and human resources was matched by timely development of checklists and guidelines to ensure high standards of care were maintained and updated with the latest evidence.
Decision-making: the usual ethical and legal considerations applied throughout. Patients were assessed for admission and treatment based on their best interests and ability to benefit, and resource limitation played no part in ICU admission decisions as regional mutual aid was always available.
As we have reached capacity, we have transferred approximately half our ICU admissions to other hospitals within the North West London Critical Care Network, which have scaled up to help cope with the significant incidence in the Harrow, Brent and Ealing population. The opening of London’s new NHS Nightingale Hospital subsequently helped to ease capacity problems. At the time of writing, we have transferred 124 COVID-19 positive patients out of 260 admitted to ICU. We hope that the UK national containment measures that started on 23 March will reduce the scale of the COVID-19 outbreak to keep within the limits of NHS ICU surge capacity.
We would like to acknowledge Vivian Sathianathan, Mike Dean, Tariq Husain, and Ganesh Suntharalingam, Consultant Anaesthetists and Intensivists at Northwick Park Hospital for their contributions to this article.
Martin Shao Foong Chong
ST7 in Anaesthetics and Intensive Care Medicine
Tun Win Hla
Giulia Sartori
ST3s in Intensive Care Medicine
Northwick Park Hospital, London
Twitter: @shaofoong @teddyhla @giulia_sartori @vivsath @Ganesh_ICM
References
- Martin D, Platt S, Hampshire P, et al. COVID-19: An update from England’s high consequence infectious diseases intensive care unit leads. [ePub ahead of print] Journal of the Intensive Care Society 2020 April 5; doi: 10.1177/1751143720918517.
- Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Medicine 2012; 38: 1647-53.
- Carenzo L, Costantini E, Greco M, et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. [ePub ahead of print] Anaesthesia 2020 April 4; doi: 10.1111/anae.15072.
- Association of Anaesthetists. Preparation for SARS-CoV-2 pandemic in South Wales: practical steps, 2020. https://anaesthetists.org/Home/Resources-publications/COVID-19-guidance/Preparation-for-SARS-CoV-2-pandemic-in-South-Wales-practical-steps (accessed 6/5/2020).
- NHS England. Specialty guides for patient management during the coronavirus pandemic. Clinical guide for the management of surge during the coronavirus pandemic: rapid learning, 12 April 2020, Version 2. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0167-specialty-guide-surge-based-on-current-hospital-experience-v2.pdf (accessed 6/5/2020).