Diary of a SAS anaesthetist at the London Nightingale Hospital
Worrying news from overseas forewarned
that hospital environments across the
country would soon be changing, and
our CEO requested volunteers for ICU
redeployment. As a SAS doctor with plenty
of recent ICU experience compared with
some consultant colleagues, it seemed
obvious to put myself forward.
Shortly afterwards, Matt Hancock announced the creation of
the 4000-bed London Nightingale Hospital at the Excel centre.
I correctly anticipated this to be my new place of work. Fear
and trepidation over the scale of the facility, and the prospect
of looking after incredibly sick patients with an incurable, highly
contagious disease, grew within me. I informed myself on COVID
management through videos, webinars and online forums. It felt
therapeutic in the face of so many unknowns.

I soon received my invitation for induction. Upon arriving, on
the official opening day, I saw Matt Hancock outside being
interviewed by a TV crew, while Prince Charles conveyed a video
message to the hospital staff. A frantic but well organised half-day
induction, delivered by a friendly and enthusiastic team, comprised
various stations: corporate induction; donning and doffing;
communication skills; proning drills; and two simulation scenarios
of critical events while wearing full PPE which was sweaty, stressful
but immensely useful. The final station, called psychological PPE,
discussed wellbeing strategies. I was amazed at how well the
programme ran, considering that the hospital had only opened
that morning.
Consultant anaesthetists were told that they would either be
supervising forty-two ventilated patients, daunting for even the
most accomplished intensivist, or be used for airway support on
specialist teams. As a senior SAS doctor, I was informed that I
would be regarded as a consultant. I mused on how easily my skills
were deemed equivalent in this context, and how different this was
to the CESR process.
Delivering effective training to highly anxious participants was uniquely challenging. The aim was to orientate and educate, and reassure not overload.
The next morning a colleague on the Nightingale induction
faculty called. The faculty were short, could I start with the
simulation training team that afternoon? I had been identified
because of my history as a simulation fellow and ALS/ EPALS
instructor, and the enthusiasm of the faculty was clearly
infectious as I agreed immediately. The faculty were friendly and
welcoming, a driven, dynamic group who got along so well that
I assumed they were old friends. In fact, they had been thrust
together very recently. Clearly, friendships and bonds were
created quickly in this fast-paced environment.
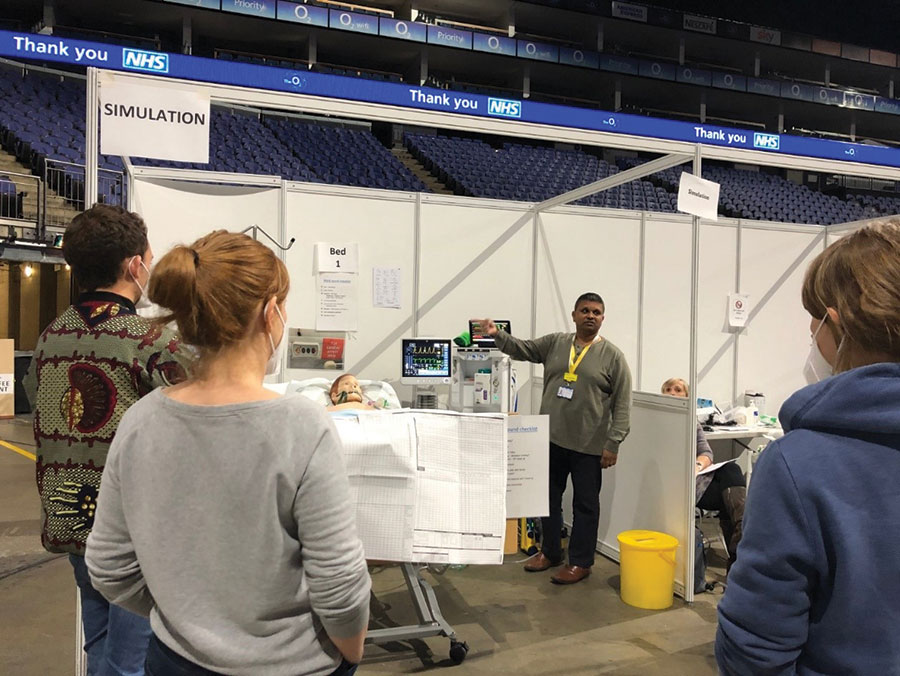
Delivering effective training to highly anxious participants was
uniquely challenging. The aim was to orientate and educate,
and reassure not overload. With groups varying vastly in
their ICU experience, we had to be agile and adaptive in our
teaching style, whilst remaining true to the learning outcomes
of the programme. Those with no ICU experience were taught
about A-to-E assessments and ICU care bundles; those familiar
with ICU were put through the critical incident scenarios. I
found that participation as a candidate was a great way to learn,
critique and implement a simulation scenario, just as being a
patient provides an invaluable insight for developing one’s own
anaesthetic techniques and communication skills.
The faculty had to combine teaching duties with clinical
commitments in their base hospitals, which often left only just
enough of us to teach the ever-increasing intake of participants
arriving each day. This made days long and relentless at
times. Equipment was also in constant short supply, though
technicians worked tirelessly to procure more supplies.
Maintaining fidelity was tricky, and required lateral thinking at
times. Despite these challenges, I felt at home within the upbeat
and energetic faculty and morale was high; we were passionate
about doing our best for this important cause and relished the
challenges that lay ahead.
These kept coming. To facilitate a massive increase in
Nightingale Hospital capacity, it was transferred to the O2
centre. We packed and moved over the Easter weekend -
weekend days and public holidays were not a time of rest.
We worked seven days in seven and, as the simulation lead
explained to us, “The hospital train is running at full speed
while the training faculty throws tracks in front of it”. That phrase
summed up the situation perfectly.
Before leaving the Excel I visited the ICU. Its vastness rendered
me speechless. I couldn’t see the end of the ward, just row upon
row of bed spaces that went on forever. The lack of sunlight,
the high roof, the ominous downlighting and the constant
rumble of the ventilation system combined to create an utterly
overwhelming experience. Birds-eye view photographs in the
newspapers gave the ward a sense of magnificence. From the
ground looking up, it was terrifying. I shuddered, hoping it
would never be filled with critically ill COVID patients.
At the O2, the vastness of the arena floor, the simulation
team’s new home, was simply breath-taking. Bed bays exactly
replicated those of the Nightingale ICU and the area was large,
imposing and noisy enough area to provide even more fidelity.
Our workload rapidly increased, and while our faculty was
expanding, I was still needed six days per week, meaning there
was no chance to take on clinical shifts. I was keen to do this
for several reasons: to help patients and staff on the ICU; to
absolve the guilt I felt for not being on the clinical front line; to
assess whether our induction had adequately prepared staff
for work on the ICU and if not, feed this back to the faculty. I
resolved to make the switch once inpatient numbers increased
as expected.
Alas, or should that be thankfully, this never happened. Just as
we were rapidly growing as a faculty, the Nightingale project
came to a surprising, abrupt end. London had coped with the
initial surge. The ward would be put into hibernation, reopening
only if needed during a second surge.
My Nightingale experience further convinced me that SAS doctors need not feel restricted by their job title or clinical duties.
I took away many lessons from my experience. I observed
effective leadership, witnessed the correlation between morale
and performance, and in an environment of flattened hierarchy
I saw how demonstrating one’s clinical, educational and
management skills conferred respect and credibility far more
effectively than one’s job title. As a SAS doctor, this heartened
me greatly, and demonstrated how a department should get
the best from all its members.


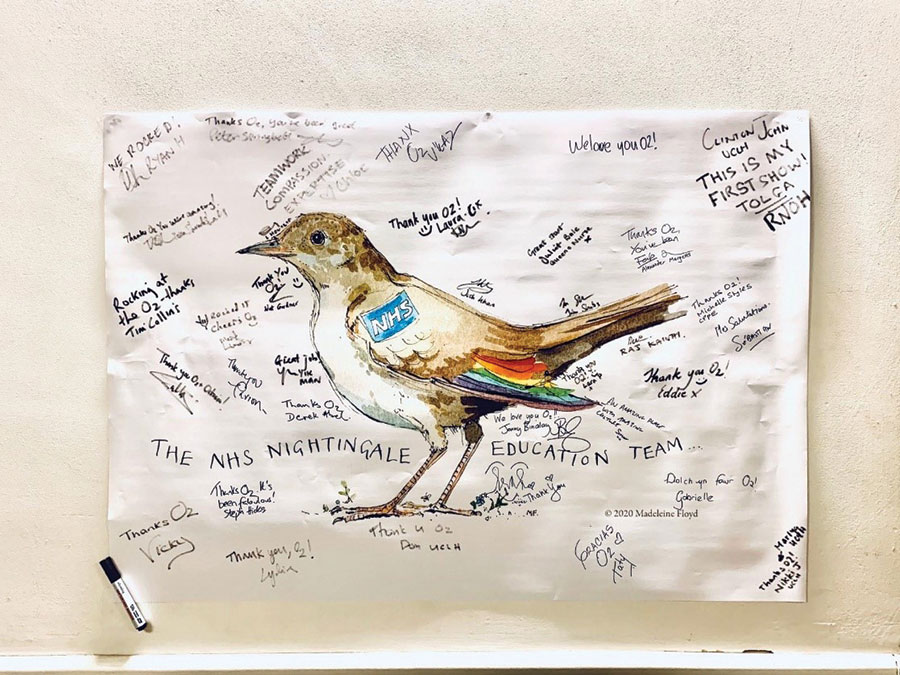
Above: Staff at Nightingale hospital
The highlights were the friendships made and the collective
sense of pride in what we achieved so rapidly at a time of
national crisis. I was delighted to receive some positive tweets
from participants regarding my teaching (the first year I shall
add tweets to my appraisal!). The conversation that touched
me most was with a participant who thanked me profusely
after a teaching session, and said that she had been inspired to
apply to medical school. To be able to recruit into the medical
profession at a time of pandemic speaks volumes.
My Nightingale experience further convinced me that SAS
doctors need not feel restricted by their job title or clinical
duties. I encourage any SAS doctor to seek educational and
departmental opportunities, and to volunteer for experiences
and positions that interest them outside their normal working
role. We all have it within ourselves to create stimulating and
multifaceted careers, and opportunities taken often result in
further opportunities arising.
I remain thankful for my Nightingale experience and look
forward to utilising the skills and experience I’ve acquired in the
future - though for all our sakes, hopefully not during a second
surge.
John Shubhaker
SAS Anaesthetist
Moorfields Eye Hospital, London
Twitter: @johnshubhaker