Safe in Sleep - a blog post from the Heritage Centre
The most cited Anaesthesia journal article in the 1950s was, Deaths Associated with Anaesthesia: A Report on 1,000 Cases, which was published in 1956, and authored by George Edwards, H.J.V. Morton, E.A. Pask and W.D. Wylie.
In 1949 the Council of the Association of Anaesthetists encouraged the voluntary reporting of deaths associated with anaesthesia. Questionnaires were distributed to all hospital groups, and the project was publicised in Anaesthesia. The authors noted above were appointed as a committee to review the returned questionnaires and the article, Deaths Associated with Anaesthesia, is an analysis of the causes of deaths associated with anaesthesia and the authors’ observations.
Given the motto of the Association, in somno securitas (‘Safe in Sleep’) it is hardly surprising that the Association commissioned this study. This study developed into the Confidential Enquiry into Perioperative Deaths (CEPOD) in the 1980s. This became the National Confidential Enquiry into Perioperative Deaths (NCEPOD) and fulfils a similar role today.
It was most likely that these deaths were caused by incorrect dosages, rather than the anaesthetic agent itself. The administration of anaesthetic by doctors who weren’t anaesthetic specialists was also a factor.
Anaesthetic death inquiries began during the 1840s in the earliest days of anaesthesia. John Snow and James Young Simpson investigated reported deaths from anaesthesia, hoping to improve patient safety. From March 1847, coroners held inquests into every “anaesthetic death.” It was most likely that these deaths were caused by incorrect dosages, rather than the anaesthetic agent itself. The administration of anaesthetic by doctors who weren’t anaesthetic specialists was also a factor.
Continued high number of deaths attributed to chloroform led the Royal Medical and Chirurgical Society (now the Royal Society of Medicine) to appoint a Committee in 1863 to investigate why this was and how it could be avoided in the future. Joseph Clover led the enquiry, which recommended that the pulse be monitored throughout an anaesthetic.
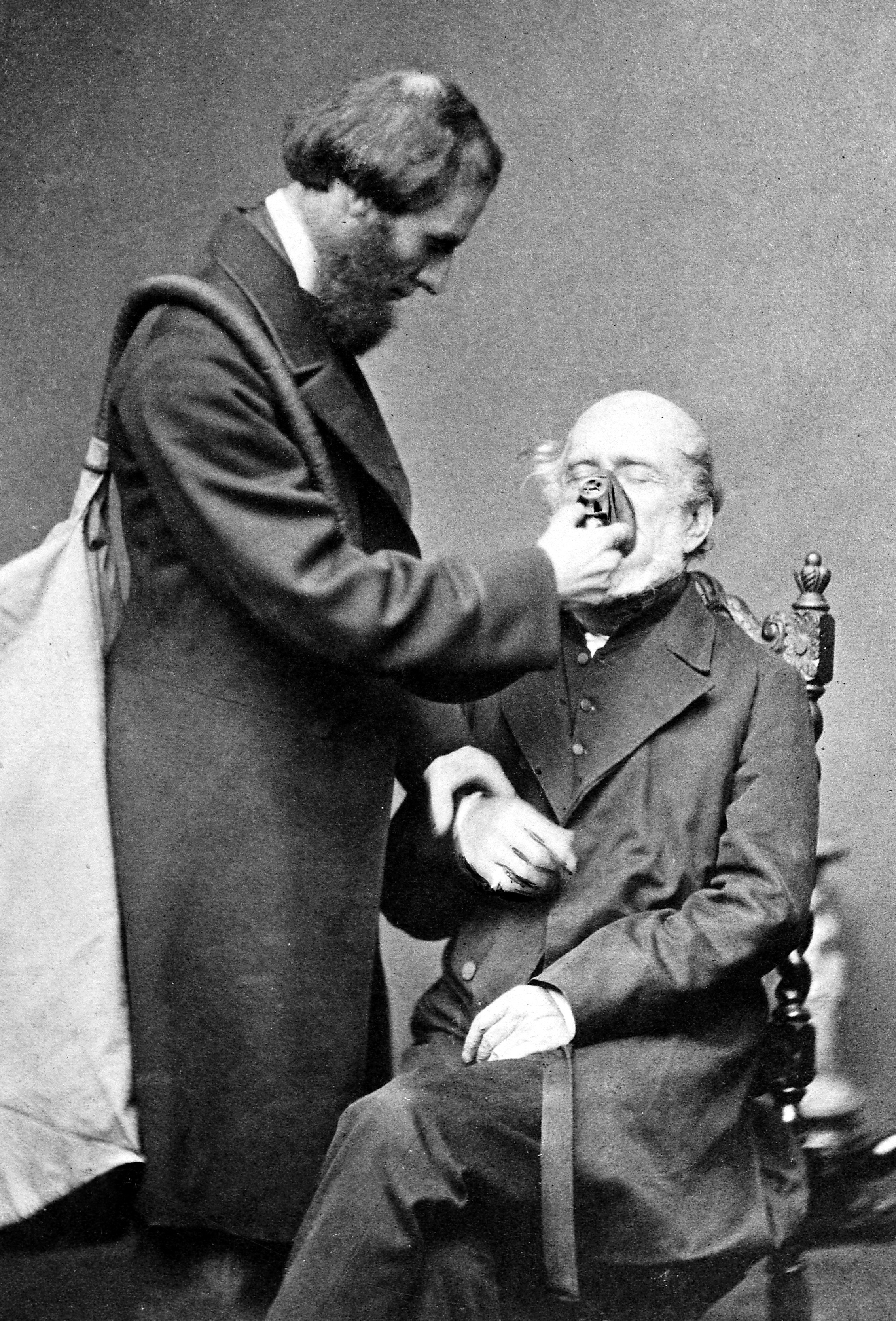
Clover with his chloroform apparatus 1862
The Royal Humane society was an early advocate of ‘training’ to reduce the number of unnecessary deaths. Concerned by the number of people mistakenly thought to be dead (and sometimes buried alive!), Doctors William Hawes (1736-1808) and Thomas Cogan (1736-1818) founded the Royal Humane Society in 1774. The doctors wanted to promote the new resuscitation technique, and even offered money to anyone who used it to try and save someone.
Their hope was to restore, ‘a father to the fatherless, a husband to the widow and a living child to the bosom of its mournful parents’.
The first meeting of the Society was held with fifteen of their friends on 18 April 1774 at the Chapter Coffee House, St Paul’s Churchyard. Their hope was to restore,
‘a father to the fatherless, a husband to the widow and a living child to the bosom of its mournful parents’.
The Royal Humane Society (then called the Society for the Recovery of Persons Apparently Drowned) set five aims:
- to publish information on how to save people from drowning
- to pay two guineas to anyone attempting a rescue in the Westminster area of London
- to pay four guineas to anyone successfully bringing someone back to life
- to pay one guinea to anyone – often a pub-owner – allowing a body to be treated in his house
- to provide volunteer medical assistants with some basic life-saving equipment
Reports reveal that mouth-to-mouth resuscitation was practiced as early as the fifteenth century, while Paracelsus was the first to experiment with bellows a century later. The bellows method was preferred by the Royal Humane Society. Their resuscitation set contained equipment that could inject fresh air or stimulants such as tobacco into the lungs, stomach, or rectum, and were located by the River Thames, London for anyone to access. The Society has kindly lent two of their kits to the Anaesthesia Museum, and one is currently on display.
The effects of putting pressure on the chest to restart the heart had been known in the nineteenth century, but although German surgeon Dr Friedrich Maass successfully used external compressions to restart the hearts of two patients in 1891, his method did not catch on at the time. Only when researchers rediscovered external compressions in 1933 did it become widely used.

Tobacco smoke enema
The first defibrillator was described in 1774 by Charles Kite. In that year, a 3-year-old child, Catherine Greenhill, fell from an upstairs window onto flagstones and, despite being declared dead, was successfully treated with electricity by an apothecary, Dr Squires. Again, it wasn’t until the 1930s that Dr W. Kouwenhoven developed internal and external defibrillation.
During the late 1950s dramatic changes took place in attitudes towards and technology for resuscitation. The new technique was to directly introduce air under pressure to ventilate the lungs. An early method was ‘mouth-to-mouth’, reintroduced by Dr Peter Safar, in which the resuscitator blew directly into the patient’s lungs, or via a tube or airway such as the Safar or the Brook. Until the 1960s, resuscitation was generally performed in hospitals. When Dr Bullough resuscitated Sylvia Berwick at the scene of a roadside accident in 1963, it was headline news.
The invention of the Ambu bag in 1956 proved to be a milestone in resuscitation equipment. Following a shortage of oxygen in Danish hospitals, Dr Henning Ruben developed the first artificial manual breathing unit, a self-inflating resuscitator and ventilation valve. It allowed the manual ventilation of the patient with room air or oxygen. Automatic gas powered resuscitators followed, such as the Stephenson and the Pneu Pac. These work off a cylinder of pressurised oxygen with an adjustable proportion of air. If connected to an endotracheal tube they can ventilate automatically, leaving the resuscitator’s hands free. They are often carried by the emergency services.