
well by an analysis of the pass rates of the American Board of
Surgery exams. For this exam, partnered men with no children
have the highest likelihood of passing. Interestingly, their
partnered female counterparts have a far reduced likelihood
of success. Married women with children have almost 30%
less likelihood of passing in comparison to their male
counterparts [4].
A recent review also recommended the entire Structured Oral
Exam (SOE) be removed entirely [5]. Therefore, are we choosing
anaesthetists based on their ability to pass an exam that will
soon be irrelevant?
Additionally, passing the Primary FRCA is just one element of
anaesthetics training and if we go back to our initial question of
‘What makes a good anaesthetist?’ I doubt it would feature on
many current anaesthetists’ list. Doctors by nature have become
adept at navigating ever-changing goalposts and will tend to
succeed at whatever is asked of them – particularly exams.
As per the most recent 2023 GMC workforce report [6],
anaesthesia has the least ethnically diverse trainee population
with over 70% white anaesthetists in training (average 49.6%).
The MSRA risks exacerbating this significant issue. Furthermore,
the RCoA’s statement that the MSRA demonstrates ‘small
differences in scores due to ethnicity and gender’ have been
proven inaccurate with Black, Asian and minority ethnic
applicants scoring on average lower compared to White
applicants [7].
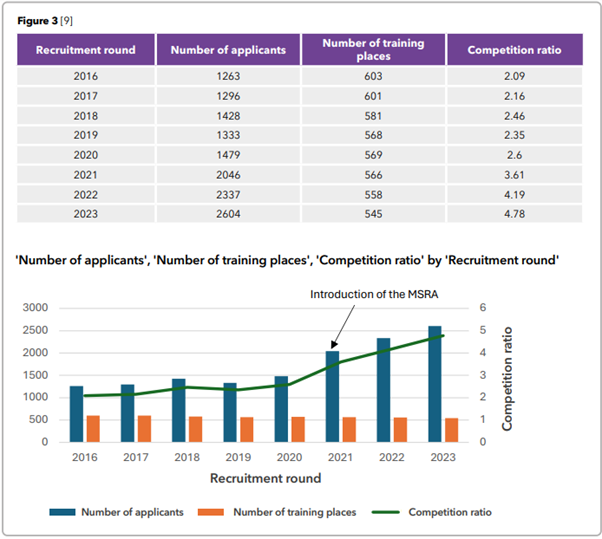
The introduction of the MSRA has counterproductively led to
a sharp increase in the number of applicants to the specialty
(Figure 3). Introduced to try and solve the issue of recruitment
workload, it has instead increased competition. It should also
be noted that while the length of the interview has also been
halved, the capacity to interview has certainly not doubled.
Given that the MSRA is valid for application to multiple other
specialties, it has encouraged many applicants (previously not
seriously interested in anaesthesia) to apply for many specialties
in one application round. As competition ratios for all specialties
grow, this practice becomes increasingly common. With most
specialties using the MSRA as a cut off to interview this leads
to the same pool of applicants with high MSRA scores being
interviewed for multiple specialties.
Despite application numbers doubling, the number of training
places has actually decreased by 10% since 2016. The RCoA has
not commented directly on this application trend but continues
to state that anaesthesia remains an attractive specialty.
Box 1
‘Experience from other specialties has
been considered, including the robust
evidence in place to support the use
of the MSRA for shortlisting for CT1
recruitment. Over 50% of all Foundation
doctors applying to core training sit
the MSRA which has been found to
have high reliability, small differences
in scores due to ethnicity and gender,
and good predictive validity in respect
to subsequent scores at interview and
performance in training. Approximately
20% of CT1 anaesthesia applicants sat
the MSRA as part of applications to other
specialties in 2019 and 2020; analysis of
this data indicates that the MSRA would
work well as a method for shortlisting CT1
anaesthetics recruitment since there is a
strong association with subsequent scores
at interview and appointability.’ [8]
Suggestions
So, if the MSRA is not the answer to the current recruitment
issues, then what is? Ultimately, applicants want a process that
is fair and rewards those with a dedication to anaesthesia.
Furthermore, an increase in training places will continue to be a
core part of the solution.
However, even if this was to occur this does not solve the issue
that we currently lack the resources to appropriately assess all
applicants. It seems there is a lack of the significant numbers
of senior anaesthetists needed to engage with the recruitment
process. Whether this is due to inability to be freed from clinical
duties, significant workload of being part of recruitment, or lack
of engagement with the recruiting bodies themselves, we do
not know
How might one improve engagement? Could the answer lie
in the recent RCoA Extraordinary General Meeting (EGM)?.
Resolution 6 outlined a strong case for regional rather than national recruitment (Figure 4) and was passed with a majority
of 88.73%. This process is likely to be fraught with complexities,
but some proposed benefits may include: